An area woman is among those charged following a statewide crackdown on Medicaid fraud that authorities say cost taxpayers nearly half a million dollars.
Jessica Fitzpatrick, 46, of South Point, was indicted this month after investigators determined she continued billing Medicaid even after she stopped providing services to a client — resulting in a $3,891 loss to the program. According to court documents, Fitzpatrick later confessed to submitting false documentation to support the fraudulent claims.
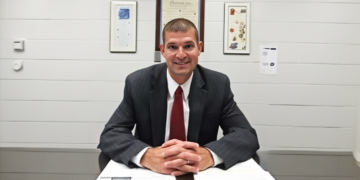
Her case is one of ten filed in Franklin County Common Pleas Court, following an investigation by the Medicaid Fraud Control Unit under Dave Yost.
Altogether, nine providers and one recipient are accused of stealing a combined $478,000 from Ohio’s Medicaid system.
“This February, remember: Love may be blind, but our investigators see just fine,” Yost said in a statement announcing the indictments. “If you flirt with fraud, your next date will be with a judge.”
Local Case Highlights Regional Impact
While most of the defendants live in northern and central Ohio, Fitzpatrick’s indictment brings the sweeping investigation close to home for Lawrence County residents.
Prosecutors allege Fitzpatrick billed Medicaid after services had ended and backed up those claims with falsified records. She admitted to investigators that the documentation was false.
Officials emphasized that Medicaid fraud not only drains public resources but also undermines care for vulnerable adults who rely on the program.
Others Indicted in the Statewide Sweep
Also facing charges:
- Destiny Allen, 26, of Cleveland – accused of overbilling Medicaid by $108,983 between 2023 and 2025. She admitted inflating hours for services never provided.
- Cheryl Austin, 53, of East Cleveland – charged after investigators calculated a $11,025 loss. Video evidence showed she never visited a client during a 20-day period she billed for. When confronted, she reportedly said, “Guilty as charged.”
- Jennifer Cavinee, 45, of Kenton – accused of billing for services not rendered, resulting in a $6,660 loss.
- Jai Dhungel, 40, of Hamilton – allegedly billed for services he did not provide, including a 20-day span with only one client visit. Total loss: $120,268.
- Shelmeta Drewery, 38, of Cleveland – accused of billing while out of state in Florida, Georgia, Nevada, and Puerto Rico. Loss totaled $4,390.
- Dejoire McAlpine, 35, of Strongsville – charged with Medicaid fraud and theft after investigators calculated a $6,587 loss. Clients reported she routinely billed more hours than she worked. She admitted submitting false claims.
- Chrishawn McClendon, 38, of Streetsboro, and William Jackson, 40, of Cleveland – accused of running a kickback scheme causing a $212,339 loss. Records show McClendon billed more than 1,000 hours while working another job and paid Jackson over $45,000 through Cash App. Both reportedly admitted to the scheme.
- Tonya Ware, 60, of Warren – allegedly billed Medicaid while traveling in Arizona, Florida, Texas, and the Bahamas. Loss totaled $4,072.
Protecting Vulnerable Ohioans
Ohio’s Medicaid Fraud Control Unit operates within the Health Care Fraud Section and works alongside federal, state, and local agencies to investigate fraud and enforce patient abuse and neglect laws.
Authorities say cases like these highlight why oversight matters — especially in rural and Appalachian communities where Medicaid services are often lifelines.
All defendants are presumed innocent unless proven guilty in court.